NCQA, the National Committee for Quality Assurance, is very clear about its mission: “We work for better health care, better choices and better health.” One tool they use to improve care is the NCQA report card program. NCQA report cards evaluate clinicians, practices, and health plans on a simple five star grading system. Since NCQA issues report cards for health plans’ networks on a state by state basis, an organization can have highly-rated networks in one location, and mediocre or poor ones in another, so it understands where to spend resources improving its networks.
But a poor score also sends a clear, cautionary message to prospective patients or providers considering joining a network. Patients with a choice between networks will obviously choose a superior one, but a similar principle applies to healthcare providers. If a network is struggling to deliver quality care, qualified healthcare providers may choose not to participate for any number of reasons: concern that their patients will not get the care they need, the risk that their ratings may be tarnished, or unwillingness to deal with red tape and administrative headaches. With fewer providers interested in a network, its quality can deteriorate further, creating a negative feedback loop.
But it can be difficult for health plans to turn such high-level report cards into action plans for improvement. Figuring out how starts with understanding NCQA report cards. What are they? How can health plans interpret the scores? And what can they do to improve their rating to retain current plan members and inspire new ones to join?
What is an NCQA report card?
NCQA explains that their report cards “help identify high-performing health care organizations. Organizations that earn a seal from NCQA show that they are serious about quality health care.” They advise that all interested parties–health plans, healthcare providers, and medical groups–should “use the report cards to find health plans, practices, clinicians or other partners that meet NCQA standards and can help you drive improvement, keep people healthy and reduce health care costs.” Clearly, NCQA intends report cards to help organizations identify opportunities to improve quality of care, its impact on patients’ lives, and deliver healthcare efficiently.
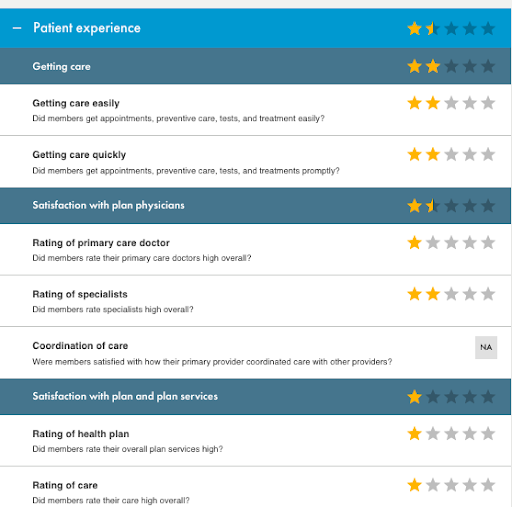
For its report cards, NCQA evaluates health plans on quality management and improvement,
population health management, network management, utilization management, credentialing and recredentialing, and member experience. Then it boils down the details and rates health plans across only three categories–patient experience, prevention, and treatment–which roll up to an overall weighted rating of between one and five stars. Organizations scoring above 2.5 stars are considered “NCQA Accredited.” The other ratings rank as follows:
- 4.5 – 5.0 stars: Excellent
- 4.0 – 3.5 stars: Commendable
- 2.5 – 3.0 stars: Accredited
- 1.0 – 2.0 stars: Provisional
It’s important to recognize that the overall rating is weighted–not an average of the three categories–and NCQA doesn’t make it clear how they calculate the weighted score. One commendable health plan clearly needs to work on the patient experience they offer:

While this accredited health plan clearly delivers an excellent patient experience:

While all three scores are important to current and prospective plan members, patient experience speaks most directly to customer satisfaction and the likelihood that a patient might choose to leave the network. Patients generally aren’t able to decide they’re receiving inadequate preventive care, or that their treatment is sub-optimal. But they are certainly aware of whether or not they’re satisfied–if they’re able to get an appointment when they want one, if they’re able to see a physician or healthcare provider they like and feel comfortable with, and if they feel the plan meets their needs.
What’s covered in the patient experience rating in a NCQA report card?
The patient experience rating in a NCQA report card covers three areas:
- Getting care
- Satisfaction with plan physicians
- Satisfaction with the plan and plan services
As with all aspects of NCQA report cards, health plans are rated on a scale from one to five stars, with five being the best. Each of these patient care areas is further subdivided into two or three criteria.
Getting care
Getting care
Satisfaction with plan physicians
Satisfaction with plan physicians uses three ratings to track members’ assessments of their healthcare providers, both primary care physicians and specialists, as well as how well patient care is coordinated between their primary care provider and all other healthcare providers.
Satisfaction with the plan and plan services
The two elements that define satisfaction with the plan are the patients’ rating of the health plan itself, meaning the services offered through the plan, and their rating of the care they receive.
How health plans can address patient experience challenges
There are straightforward ways that a health plan can address poor ratings for its patients’ ability to get care and their satisfaction with their physicians. Health plans can improve their ratings for access by identifying additional qualified providers and adding them. If patients are dissatisfied with their experience with their physicians, networks must do a better job vetting providers before recruiting them into the network.
These problems can be traced to a mindset that focuses solely on meeting CMS’ requirements for adequacy, rather than recognizing that satisfied patients, receiving quality care, will ultimately determine the success or failure of a network. But health plans have many other operational requirements they must meet beyond building the strongest possible network in a given market. They have multiple plans in multiple geographies to manage, market to patients, and process payments; strategic growth targets to plan and measure performance against, and more.
“
The temptation to reach adequacy and go to market is strong, but building to a higher standard can lay the foundation for a positive patient experience.
”
Building a strong provider network that exceeds the minimum requirements means patients are more likely to find providers they enjoy working with–and that’s the easiest way to earn high marks for patient satisfaction. The most efficient way for a health plan to do this is to partner with an organization that has demonstrated skill and efficiency at network development and credentialing, two time-consuming and detail-oriented tasks.
A more strategic approach to network development, in which a trusted partner understands the requirements of adequacy and how they play out in a given geography, can improve patients’ access to care by building stronger networks from the start or upgrading existing networks. Having a rich database of provider data and ongoing network monitoring can ensure that a network consists of highly-qualified, credentialed providers who provide quality care to patients.
The path to building a strong healthcare network isn’t always a straight line. A poor NCQA report card doesn’t necessarily lead to its failure–but health plans have to understand what it means and determine whether they have the ability to remedy their plans’ shortcomings or need to turn to a partner for help.