Credentialing plays a critical role in helping ensure that patients receive quality care from fully qualified professionals. Whether a provider applies to join a particular healthcare network or the network recruits the provider, the health plan–or any other healthcare payor offering services–must verify the provider’s credentials. Because of the legal and regulatory consequences that could ensue from healthcare decisions and procedures being made by under-qualified providers, health plans (or other payors) are responsible for verifying:
- What kinds of qualifications (i.e., education and training) their providers have
- Whether their providers have kept their knowledge up-to date with continued training
- Whether other institutions the providers are associated with can corroborate these facts
Traditionally, credentialing is a time-consuming manual process. Providers complete and submit their applications manually (or have administrative teams do so for them). Then the health plan’s credentialing team, whether in-house or outsourced, goes through the application, painstakingly validating providers’ educational background, training, employment history, and state licenses and many other details. The credentialing process may include background checks, identifying previous disciplinary measures, and checking for current sanctions or exclusions, as well. The verifications often require making phone calls, filling out forms, sending faxes and emails, then tracking the status of all of these requests and following up if responses are not timely. By its nature, the credentialing process takes time to complete thoroughly for one provider, but no organization credentials one provider at a time.
They must credential each of the thousands of providers in a given network.
For each of the thousands of healthcare provider networks across the country.
It’s no wonder healthcare administration is awash in red tape and bureaucracy.
Issues with manual credentialing
When all these processes are performed manually, a number of issues arise throughout the entire credentialing process, affecting not only health plans, but also providers and ultimately patients. Medical practices spend, on average, $7,000 for each provider credential application, plus 20 hours of administrative time. Since the processes are manual, they are prone to human error. Administrative workers will occasionally enter a telephone number, email, or address incorrectly. This wastes the health plans’ credentialing teams’ time, which leads to delays in approvals for providers, who may spend months on staff before they’re able to see patients–impacting practices’ bottom line and patients’ ability to receive care.
“
What happens when a document is missing, or a practice moves locations, or a license expires, leading to delays in employment verifications? More of the same, unfortunately.
”
Despite these issues, no one is suggesting we do away with credentialing. Patients deserve quality care, and credentialing plays an important role in ensuring that qualified providers do so. But the process is certainly ripe for improvement. Automating credentialing–or as much of it as possible–can reduce human error and eliminate delays between steps. It can make credentialing more efficient across the entire process, from application to completion of the final primary source verifications.
Automating provider credentialing applications
How might automation make credentialing applications easier for providers? What if organizations or providers could start the process through any of a number of convenient ways–by providing their CAQH credentialing data, submitting their own data, through an application programming interface (API) that allows organizations to automate submissions from their proprietary data sources, or using a simple online application? What if the application drew on an industry-leading database of provider data to supplement the application with verified data, reducing the risk of inaccurate submissions?
The andros application system is designed to make providers happy. In fact, most of our credentialing applications don’t require any provider input. Whether we receive data from a client through an API, batch upload, or the provider-filed application, that step triggers the credentialing process and alerts andros to validate the providers’ data in its NCQA-certified credentialing process.

Our robust repository of data in the a* platform helps autofill provider information from verified sources, so that it’s nearly impossible for incorrect information to be submitted. In the 20 minutes it takes to complete, our application takes the burden off of your team and the providers in your network.
Automating credentialing primary source verifications
Once the application is complete and submitted, in a traditional manual credentialing workflow, the professionals begin verifying that the information submitted is accurate and complete by reaching out to the appropriate institutions, employers, and licensing boards. andros automates physician credentialing in two ways: by developing, maintaining, and continuously validating large stores of provider data and by implementing automated, low-touch workflows.
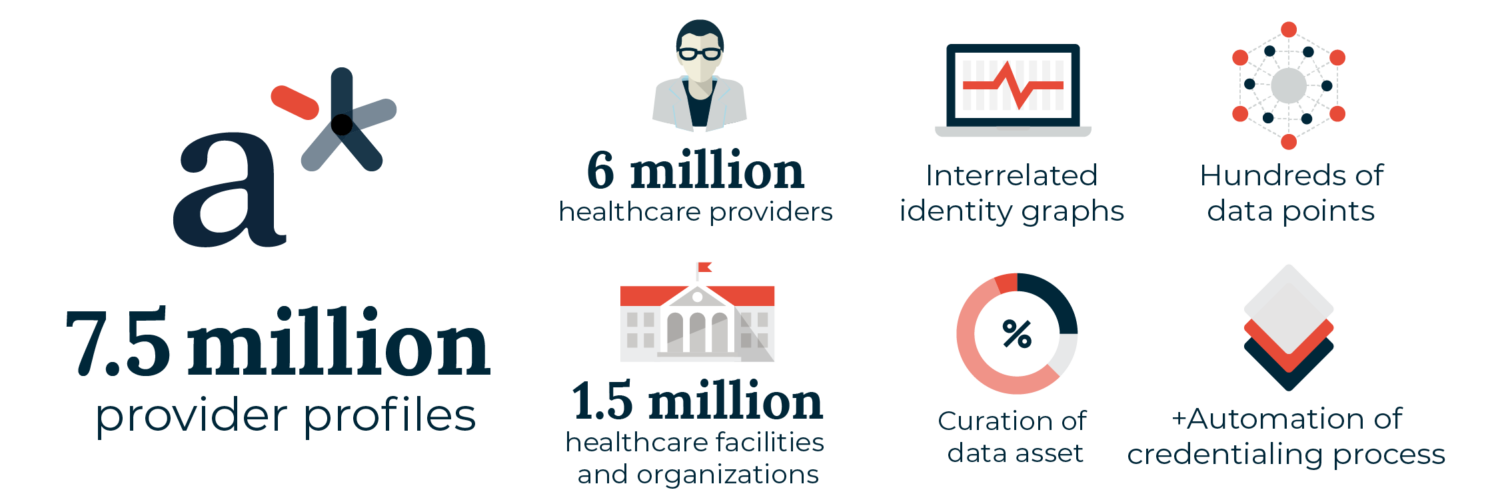
The a* platform, the largest single healthcare provider database in the industry, contains validated data on over 7.5 million providers across the United States. As andros collects data points from educational institutions, state licensing boards, federal databases, regulatory entities, and more on every provider we recruit, contract, or credential, the a* platform validates the new and existing data, increasing its accuracy and usefulness across the board.
During credentialing workflows, the a* platform uses data-matching algorithms to automate primary source verifications, identify gaps in the required information, and flag potential roadblocks like licensing issues or sanctions. If the a* platform can’t resolve the discrepancies, then it is routed for professional outreach to help resolve any issues. The andros team digs in on behalf of clients, reaching out to providers and facilities at least three times to get to the bottom of any flagged issues and perform quality checks to ensure every credentialing report is up to NCQA standards.
Primary source verifications (PSVs) tracked by andros include:
- National Provider Identifier
- State medical license
- DEA and/or CDS license
- Board Certifications
- Sanctions and exclusions
- Malpractice History and any disciplinary information
- Education verification
- Medicare opt-out
- Optional PSVs like the Social Security death master, hospital admitting privileges, and ad hoc state licenses
- Medicare and Medicaid exclusions through NPDB query
Automated credentialing reporting
“
Digital data may be more valuable as it can be transferred from system to system for other purposes.
”
Credentialing isn’t complete until all the t’s have been crossed and i’s have been dotted. Health plans may want PDF copies as documentation of the process, but in many cases, digital data may be more valuable as it can be transferred from system to system for other purposes.
With andros, after credentialing is complete, clients receive all the provider information in an easy-to-read profile, including vital information like specialty, languages, malpractice information, credentialing status and much more. With comprehensive credentialing reports provided in multiple formats–PDF downloads, the andros web portal, or automated API transfers–clients can move through the final review and approval processes efficiently (or allow andros to manage the Credentialing Committee process as well).
Find out more about healthcare provider credentialing with andros.