The 90 days plus time taken [for credentialing] is not acceptable. No one at the insurance company is available… emails are not responded to for many many days… talking to different people has no results.
-Anthony D., healthcare provider
When you ask a consumer what they think of the experience of procuring and receiving healthcare, chances are you’ll hear some negative feedback. Delays in receiving care, uncertainty over costs, and confusing billing and reimbursement processes all negatively impact patients’ experience of healthcare. As much as regulators and payors want to focus on health outcomes, the experience matters to patients. Recent surveys have shown patients care more about customer service and communication with their healthcare providers than things like bedside manner.
The same is true of healthcare providers. The frustrating combination of administration, bureaucracy, and delays that starts with providers’ and health plans’ very first interactions during the credentialing process diminishes provider satisfaction. To maximize market share, health plans should prioritize improving the provider experience, for the benefit of providers, patients, and regulators. Ensuring that their healthcare providers are satisfied and happy to be partnering with the health plan produces a positive feedback cycle that benefits patients as well–and this begins with provider credentialing.
The impact of credentialing delays
Credentialing turnaround time impacts patient access to care, most critically, as well as our bottom line. The sooner our providers are credentialed and able to see patients, the sooner those patients can get the care they need and the sooner we can bill for our providers’ services.
-Lori H., health plan professional
When credentialing processes are complicated, burdensome, and prone to delays, health plans, providers, and ultimately patients all lose out. Excessive bureaucracy, poor communication, and prolonged timelines lead to gaps in network coverage, dissatisfied providers, and patients’ not receiving the care they need on time.
Both providers and payors want the credentialing experience to be better. For providers, it’s the first impression that they have of the payor–and it’s generally not a good one. There is a misconception that payors don’t care about the provider experience. However, this is not the case. The more providers are satisfied with a given health network, the more likely they are to stay and recommend it to others.That ensures that the network is robust and able to meet patients’ needs on a timely basis–which in turn keeps their patients happy and impacts their bottom line.
In an effort to learn more about the provider experience during the credentialing process, andros conducted an extensive survey of providers in California, Florida, New York, and Texas. Our intent was to better understand the initial administrative experience that providers have with health plans and the friction points that cause them to have a bad experience.
A neutral provider experience isn’t good enough
Some good news out of our survey is that more providers were satisfied with their credentialing experience than were actively “not satisfied.” The bad news, though, is that far more respondents rated their experience as “neutral” than were either satisfied or dissatisfied. In total, only 29% of providers were satisfied with their credentialing experience, where 70% found it neutral or unsatisfactory.
Considering that most providers are expecting delays, red tape, and bureaucratic headaches, that’s a poor result. If you head out for dinner, would you be satisfied with a restaurant that “wasn’t bad?” If you decide to see a movie on Friday night, would you be excited to see a movie that earned two stars out of four? Why then is it surprising that providers, who already have low expectations of the credentialing process, aren’t excited to join new health care networks.

Time is the most critical factor in provider satisfaction
Credentialing turnaround time is very important as the sooner I can get credentialed, the sooner I can see those related patients.
–Charles K., healthcare provider
Time is of the essence here. Doctors make their living by seeing patients right away. Therefore, it is crucial to finish their credentials as swiftly and effectively as possible.
-Ellynor H., health plan professional
Credentialing turnaround time is very important since we have patients who are waiting for important drugs or procedures.
-Nilanjana B., healthcare provider
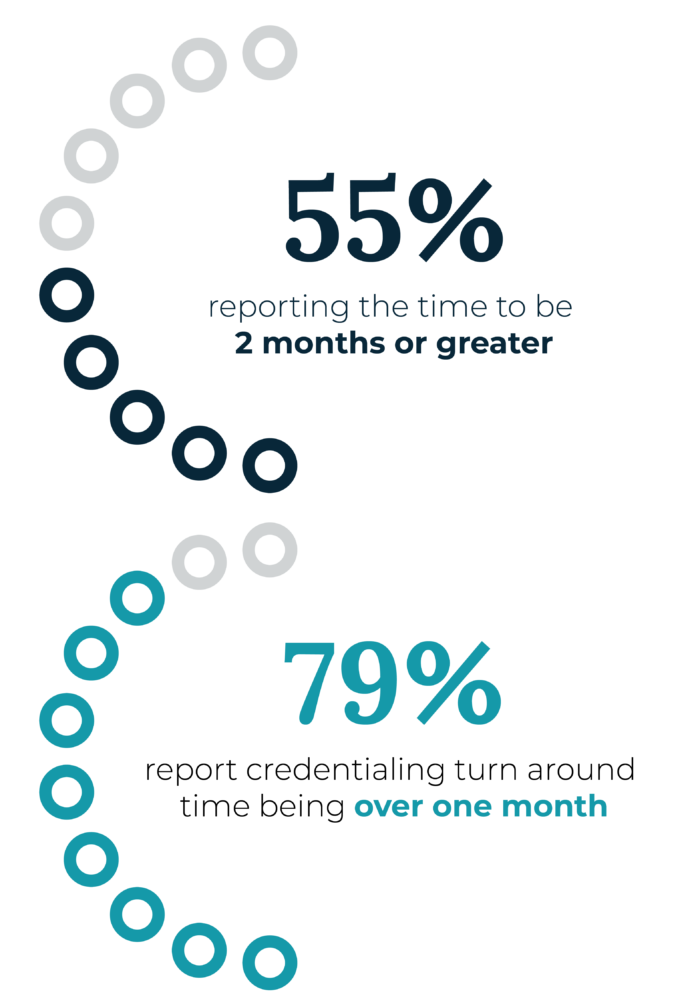
Digging deeper into the issues around provider satisfaction with the credentialing process reveals the biggest factor is turnaround time. Our survey revealed over half of providers (55%) report waiting more than 60 days for their credentials to be approved. Almost four in five (79%) are waiting more than a month. These delays don’t just impact providers. They also have negative impacts on health plans and patients.
Healthcare providers are effectively sidelined while waiting for their credentialing applications to be approved. When they’re unable to see patients, they’re not only missing an opportunity to generate revenue for the practice, but also the opportunity to deliver timely care to patients in need. Health plans run the risk of underperforming on STARS and other regulatory measures related to member health outcomes, timely access and availability to providers, and customer services to name a few reasons.
The causes of credentialing delays
You could certainly dedicate an entire article to exploring the challenges that cause delays and errors in credentialing–and actually we have, if you’re curious. But that’s not our goal in this article, so we’ll just cover the topic at a high level.

The primary cause of delays in credentialing is the primary source verification (PSV) process. Every detail of a healthcare provider’s background and experience–job history, qualifications, formal education, training, certifications, licenses, etc.–must be checked and validated before the health plan can approve the provider’s application. This takes time–usually one month–but all too often it takes two, three, or more months. These delays crop up because of a variety of reasons, ranging from data entry errors and typos to outdated contact information and even deceptive intentions.

The second cause of delays is the approval process most health plans use. A health plan’s credentialing committee must meet, usually on a monthly basis, to review healthcare providers’ applications and approve them before the providers can render services to patients under that particular health plan. And just like PSVs, for many health plans these committees are plagued by administrative delays–just think about the headaches involved with scheduling several busy physicians to meet for several hours and review hundreds or thousands of credentialing applications!
Improving providers’ experience of credentialing
Health plans are missing an opportunity to delight providers and build stronger networks. Delays in the process cost providers and health plans money, while crucially impacting patient health outcomes as well. But what can be done? The biggest factor in provider satisfaction is the speed of the credentialing and approval process. Partnering with andros can accelerate credentialing turnaround times in a number of ways.

Make credentialing applications simpler and faster. andros eliminates barriers by allowing providers to start credentialing three ways: by providing CAQH data, by providing provider data, or through the andros provider application. Health plans can accelerate credentialing even further using the andros API to automate submissions, as well.

Leverage provider data to improve process efficiency. andros helps reduce delays and approve providers quickly using the provider data in the a* platform. Our industry leading primary source verification turnaround time moves providers with compliant applications through the process rapidly, completing credentialing up to 10x faster than industry standards.

Rectify application errors quickly. When applications are missing or have incorrect data, andros identifies errors and rectifies them with data that is consistently retrieved and validated from primary sources. When that doesn’t work, our solution automatically reaches out to flagged providers to ensure applications are complete and compliant.

Consider outsourcing credentialing committee administration. Focus on making decisions, not the headaches associated with running a credentialing committee.
Take a deep dive into the provider experience with our ebook Creating a Better Provider Experience.