“
Primary care providers are more interested in acquiring new patients with their existing health plan contracts then they are in signing contracts with additional health plans
”
andros executed our Q3 Provider Market Study to better understand primary care provider sentiment around network contracting and access to specialist providers for their patients. Part of what compelled us to focus on this topic was industry feedback on network impact to member enrollment.
Key takeaways from this study support the conclusion that
Primary care providers are more interested in acquiring new patients with their existing health plan contracts than they are in signing contracts with additional health plans.
- 85% of primary care providers andros studied report that they are accepting new insured patients.
- 65% of the providers reported they are only interested in adding 0-2 new health plan network relationships over the next three years. This leave only ~⅓ of providers interested in expanding by at least 1 network relationship per year.
- Providers interested in new contracts prioritize adding Group Commercial, followed by Medicare Advantage, ACA, and lastly Medicaid Managed Care.
Key Takeaway #1
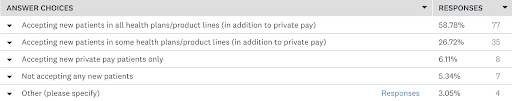
85% of primary care providers andros studied report that they are accepting new insured patients.
91% of respondent PCPs reported accepting at least some new patients (including 6% reporing only accepting new cash payment patients). Of those accepting new patients, nearly 60% have open panels for all of their contracted networks, and another 1 in 4 are accepting new patients in at least some of their contracted products.
Key Takeaway #2
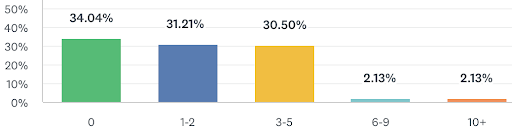
65% of the providers reported they are only interested in adding 0-2 new health plan network relationships over the next three years. This leave only ~⅓ of providers interested in expanding by at least 1 network relationship per year.
A full ⅓ of the providers reported they are not interested in joining any additional networks in the next three years, and a similar amount are looking to add less than 1 new contract per year. The remaining ⅓ are seeking more aggressive contracting growth with the majority adding a total of 3+ contracts over a 3 year period
Key Takeaway #3
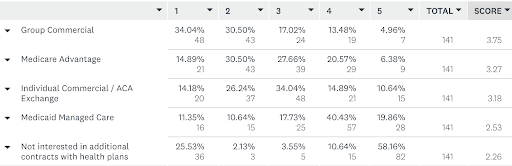
Providers interested in new contracts prioritize adding Group Commercial, followed by Medicare Advantage, ACA, and lastly Medicaid Managed Care.
These responses follow a similar pattern of providers reporting they prioritize reimbursement rates when making contracting decisions, as Group Commericial is often the highest reimbursed line of business and Medicaid Managed Care the lowest.