
Humana, the third-largest health insurance provider in the country, attempted to handle credentialing internally, but soon recognized their large provider network was too big to handle themselves and that they needed to outsource to a CVO.
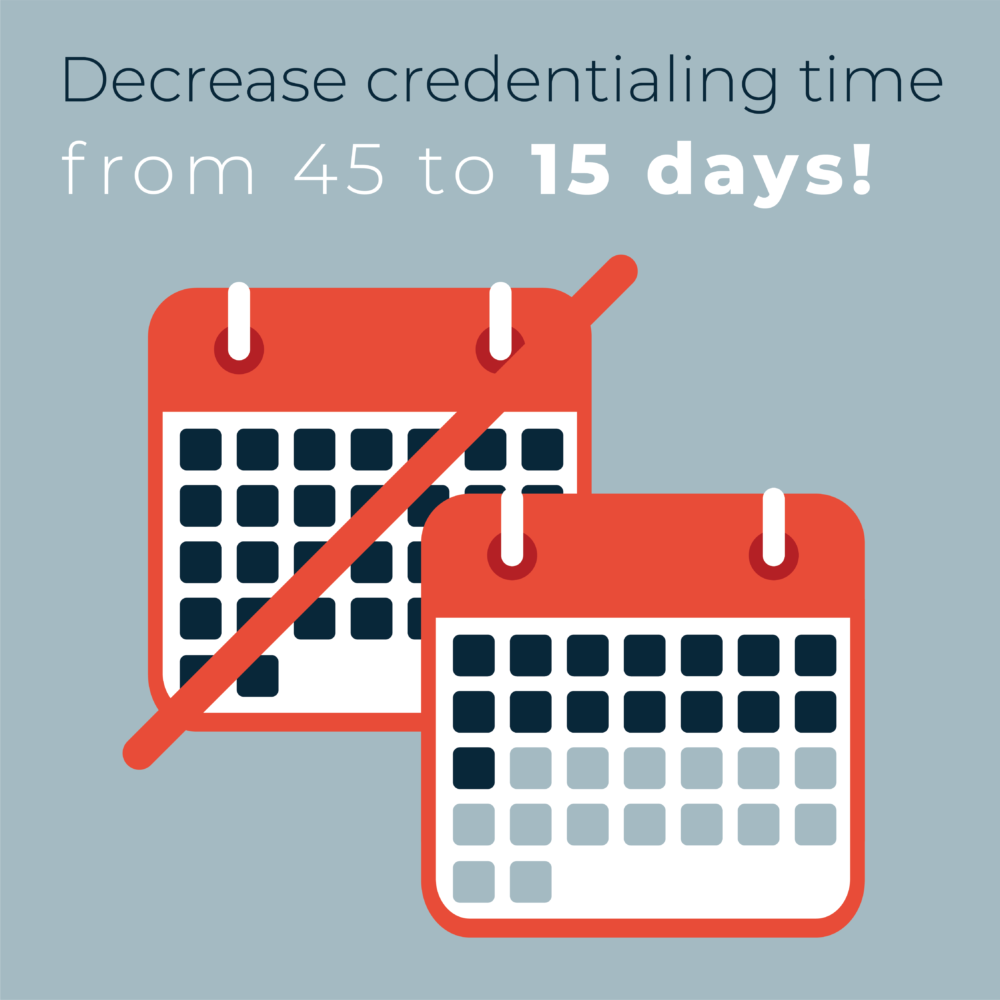
However, after 5 years Humana wasn’t satisfied with the vendor they had chosen – slow turnaround times of over 45 days were plaguing their networks, and troublesome regulatory penalties were causing additional headaches.
There had to be a better way.
When Humana began searching for a new CVO partner, they had clear criteria – their next vendor had to be a long-term solution to their problems. They needed an organization deeply-rooted in industry knowledge, with a strong reputation and great RFP responses.
This criterion demanded that Humana’s search process be highly selective. They couldn’t afford to spin their wheels with a second CVO partner – this one had to work. As they were vetting potential candidates, a recurring issue arose – no one shared a partner-oriented approach. Until they met andros.
The andros approach was all about the journey to success, one that would be paved with a commitment to partnership. Unlike the other vendors, andros was the only CVO who offered a dedicated Client Success Manager to Humana. And after speaking with our robust list of client references, who reinforced Humana’s confidence in andros, a partnership was born.
Our unique approach enabled Humana to proactively identify potential
compliance issues and mitigate them before consequences arose.
Offering comprehensive, end-to-end healthcare provider network management services, including recruitment and contracting, credentialing, and provider data management.