The increased demand for nurse practitioners (NPs) and physician assistants (PAs) is a nationwide trend that is expected to continue over the coming years. The U.S. Bureau of Labor Statistics expects a growth of around 19% in nurse practitioners alone by 2020 — well above the national average.
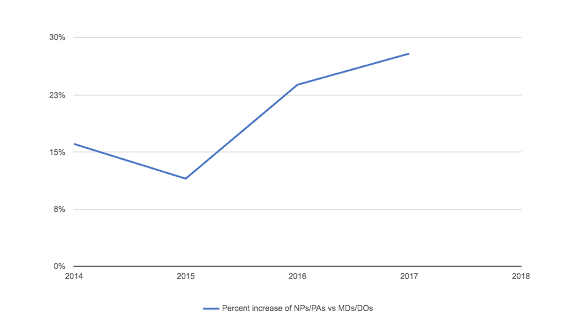
We’ve seen this trend reflected in an increase in the ratio of PAs and NPs we’ve credentialed over the last 4 years compared to MDs and DOs. As this chart shows, the ratio of credentialed NPs and PAs over the last 4 years has increased by more than 10%.
There are many factors contributing to the increased demand for PAs and NPs. Healthcare organizations are expanding to meet the needs of the growing healthcare consumer base. With the Affordable Care Act, more people are accessing healthcare for the first time. Healthcare organizations are hiring NPs and PAs to fill in the provider-to-patient gap because they are more cost-effective than physicians. With specialized training, the ability to see patients without a physician, and the power to prescribe medication (in most states), NPs and PAs are seen as a solution for properly staffing clinics and hospitals because they help increase patient care with a lesser impact on overall costs.
All these factor combine to increase credentialing for PA and NPs at the healthcare facility level and at the payer level.
The Impact on Your Credentialing Process
Dr. Garry Choy, chief medical and compliance officer and andros cofounder, underscores why it is so important to understand the nuances of credentialing allied health professionals, “PAs and NPs are critical frontline healthcare providers with extensive and increasing responsibilities in patient care. They are needed more and more to help address growing volume of patient visits and healthcare utilization. Hence, it is imperative that credentialing PAs and NPs should be of the highest efficiency, quality and accuracy.”
Yet there still is a lot of confusion surrounding the credentialing process for these health professionals due to the different levels of credentialing required.
[cta id=”contact”]
How an NP or PA is credentialed is dependent upon how they are contracted. If they are practicing as an independent practitioner — meaning they are able to see and treat patients without supervision from physicians — health plans will need to verify their credentials based on NCQA requirements (CR1). This means checking education and training, which includes board certifications. However, if PAs and NPs are not working independently, from both a payor and facility perspective they do not need to be credentialed, and therefore board certification does not need to be verified. However, this may still depend on the policy and procedures of the health plan and local healthcare facility. It still may be a good idea to credential these providers and go above and beyond the most basic requirements to further demonstrate that the NPs and PAs on staff have the appropriate training and background (JCO HR 1.02.05).
Further, the board certifications for PAs and NPs not only vary from physicians, but there are two main certifying boards for NPs that cause additional steps in the verification process. These differences only increases the workload for credentialing NPs and PAs.
andros helps health plans navigate these nuances. Not only that, our technology allows us to drastically decrease turnaround time by removing a lot of the manual credentialing work (all while increase data accuracy and compliance).
Contact us to learn more.