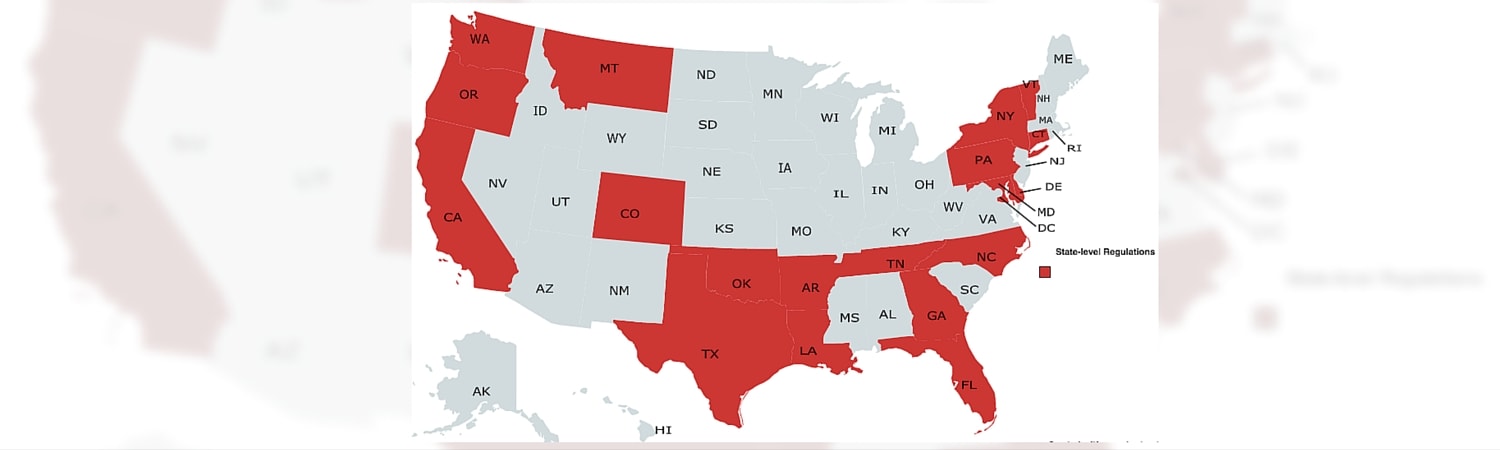
Provider directories have long been a source of inaccurate provider information. As a result, federal (CMS) and state regulations will be enforced to ensure that healthcare consumers receive accurate information. Failure to comply with these specific state regulations will result in certain penalties.
Stemming from work with health plans throughout the United States, our compliance team compiled a list of regulations for each state.
State Regulations
| State | Regulation | Health Plan | Link to Official Content |
|---|---|---|---|
| Arkansas | Must update directories every 14 days | All | Click here |
| California | Must update online directories weekly | All | Click here |
| Colorado | Must update directories monthly | QHP | Click here |
| Connecticut | Must update directories annually | MCO | Click here |
| Delaware | Must update online directories annually | QHP | Click here |
| Florida | Must update online directories semi-annually | EPO | Click here |
| Georgia | Must update online directories every 30 days | MCO | Click here |
| Idaho | Must update directories monthly | QHP | Click here |
| Louisiana | Must update directories annually | All | Click here |
| Maryland | Must update online directories every 15 days | All | Click here |
| Montana | Must update directories annually | QHP | Click here |
| Nevada | Must update directories every 30 days | QHP | Click here |
| New Jersey | Must update online directories every 10 days | MCO | Click here |
| New York | Must update online directories every 15 days | HMO | Click here |
| North Carolina | Must update directories annually | All | Click here |
| Oregon | Must update online directories monthly | MCO – Workers Comp | Click here |
| Tennessee | Must update directories annually | MCO | Click here |
| Texas | Must update directories quarterly | EPO, HMO, PPO | Click here |
| Vermont | Must update directories semi-annually | MCO | Click here |
| Washington | Must update directories monthly | All | Click here (Subchapter B) |
| Wisconsin | Must update directories annually | HMO | Click here |
Beyond the proposed timeline of updates, states have also released their expectations for provider directory content. If you would like to learn more about these specific requirements please contact us.
No State Regulation
Where there are no state requirements, the following CMS guidelines must be followed: Provider directories must contain relevant and accurate provider information. This will be implemented through directory maintenance through monthly updates of provider information and quarterly touch points with providers within a Qualified Health Plan network.
| State Name | Regulation | Health Plans | Link to appropriate CMS letter |
|---|---|---|---|
| Alabama, Alaska, Arizona, Hawaii, Illinois, Indiana, Iowa, Kansas, Kentucky, Maine, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Mexico, North Dakota, Ohio, Oklahoma, Pennsylvania, Rhode Island, Utah, Virginia, West Virginia, Wyoming | Must update provider directories monthly and collect up-to-date information from providers quarterly | QHP & Medicare Medicaid | Guidance to Verify that Networks are Adequate and Provider Directories are Current (p. 134-135) |
With the recent demand for transparency in healthcare, specifically in provider data, CMS federal regulations have been put in place to promote efficiency within the healthcare system. State regulations have begun to fall in line with this nationwide agenda. Thus, it is clear that no state is free of regulations pertaining to provider directories, and most states are aligning themselves with federal regulations.
Explanation of Acronyms
MCO – Managed Care Organization: Health plans that provide health care in return for a monthly fee and coordinate care through a defined network of physicians and hospitals. Examples of this include HMOs, PPOs and EPOs.
HMO – Health Maintenance Organization: Under this plan, enrollees have one primary care physician and need a referral before they can see any other healthcare professional, except in an emergency.
PPO – Preferred Provider Organization: Enrollees can go to any healthcare professional without a referral inside or outside a health plan’s network.
EPO – Exclusive Provider Organization: Enrollees have a limited network of doctors and hospitals to choose from, which is set by a health plan. It is important for enrollees to know who participates in their plan’s network
QHP – Qualified Health Plan: Designation given to health plans that are sold in the marketplace under the Affordable Care Act (ACA)