Organizations of all sizes have struggled to solve the challenges of building healthcare provider networks, especially for Medicare Advantage, on schedule and on budget. Healthcare organizations have to analyze patient demographics and local geography, then make wise choices where to invest. They need to comply with complex regulatory requirements and demanding timelines.
But despite these geographic and regulatory challenges, provider data poses the biggest network development challenges to healthcare organizations. Provider data challenges span the entire network development process, from recruiting and contracting providers through credentialing and even monitoring the network after it is in market.
Provider Data Challenges During Recruiting
During recruiting and contracting, inaccurate and incomplete provider data translate directly into wasted time and energy. An organization may identify key providers they need to reach adequacy, but if they don’t have the right contact information–or even if they have incomplete information–its recruiters may not be able to contact them to determine if they’re available or interested in joining the network. Even if the provider is interested, incomplete or inaccurate data can result in a contract being mailed to the wrong location, bouncing from an outdated email address, or even sitting in an outbox next to an unattended fax machine(!).
“
Having inaccurate data can lead to a substantial waste of resources if a healthcare organization pursues a network build when it was unlikely to achieve adequacy in the first place.
”
The fact that provider data is constantly changing compounds the challenge posed by inaccurate and incomplete information. Providers retire, switch practices, change careers, or move across the state or even the nation–but their data doesn’t always keep up with them. This exacerbates the challenges recruiters have, as they may be working from data that the provider forgot to update or didn’t know existed in the first place. And these issues have only increased in the past two years, as the healthcare industry has been subject to the “Great Resignation” just as much, if not more than, other industries.
Inaccurate data–about the location of a provider’s office or a healthcare facility–can be especially problematic in Medicare Advantage network builds. With complex adequacy regulations requiring that a certain quantity of providers be located within a certain distance of patient populations, having inaccurate data can lead to a substantial waste of resources if a healthcare organization pursues a network build when it was unlikely to achieve adequacy in the first place.
Provider Data Challenges During Credentialing
Once an organization turns to credentialing a network, the diversity of sources for provider data becomes the biggest challenge. To ensure they get an accurate picture of a provider, organizations must pull data from a variety of sources, including educational institutions, past and current employers, licensing entities and regulatory agencies, all of which may be scattered within and outside of the area where the network is located. Credentialing professionals must reach out to each of these data sources–and potentially experience the same issues with inaccurate contact information, or an inaccurate NPI, or a provider whose name has changed, and so forth. All these issues introduce delays in credentialing that could result in missing a key deadline in the network development process.

The Solution to Provider Data Challenges
Given the challenge posed by inaccurate, incomplete, outdated, and disparately-sourced data, the solution is having a “single source of truth” for provider data. Unfortunately, for healthcare organizations, developing and maintaining such a data resource isn’t practical. Their energy, time, and expertise is better spent building networks, managing payments and reimbursements, and ensuring their patients receive quality care. It’s more efficient to partner with an organization that is skilled in network development and credentialing and possesses deep insight into provider data–like andros.

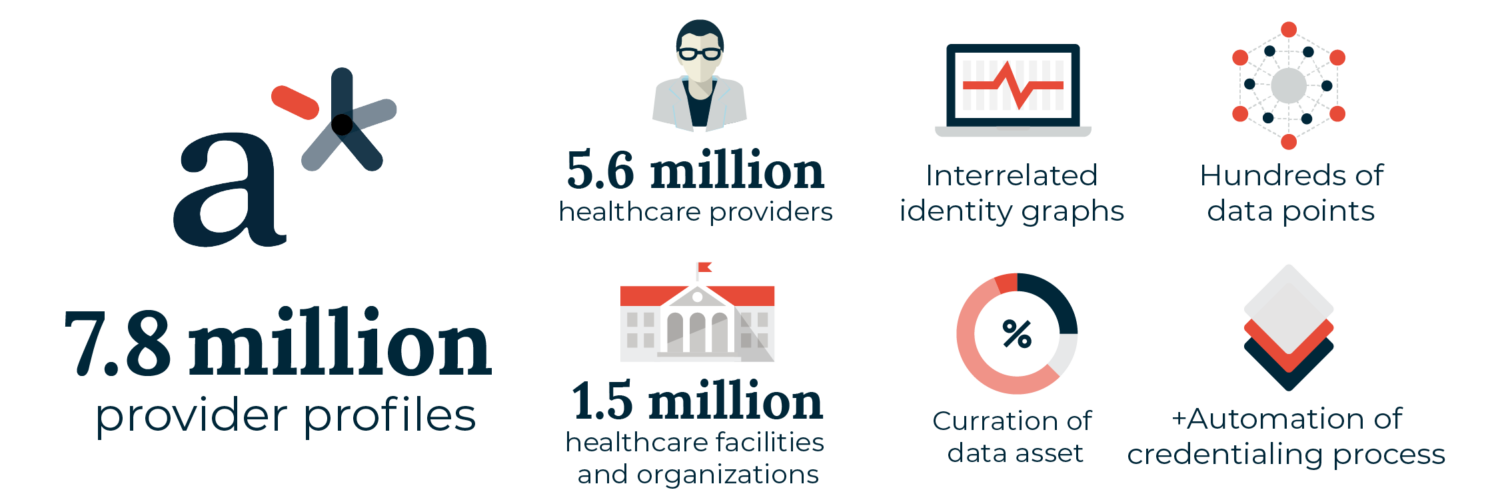
As andros builds the leading healthcare networks in the country, we collect data points from educational institutions, state licensing boards, federal databases, regulatory entities, and more on every provider we recruit, contract, or credential. As they are added to the a* platform, we validate the new and existing data, increasing its accuracy and usefulness to all our clients. With over 7.8 million data points on healthcare providers and facilities, the a* platform is the healthcare industry’s preeminent provider database. As the brain powering the andros technology suite, the a* platform layers intelligence and workflows over an unparalleled data resource, replacing the previously manual processes used to build and manage provider networks with optimized digital workflows.
Find out how andros can help you solve your provider data challenges by reaching out to a representative today.