AI has become impossible to ignore, with its influence rippling across nearly every industry. That’s for good reason—its potential to change how we work is real. But in healthcare, especially in provider network management, there’s also real apprehension. The term “AI readiness” often triggers questions about risk, compliance, or job displacement.
At Andros, AI readiness isn’t about going from zero to total automation overnight. It’s about building confidence and competence with the right foundation—starting with low-risk, high-impact use cases that enhance human decision-making and help teams work smarter, not harder through every stage of the network lifecycle.
We think of AI readiness not as a leap, but as a progression. We’ve been talking about this with many of our clients and thought it was time to illustrate how health plans that are ready can take the first step.
Why AI readiness matters for provider network management
Currently, most of the AI being used successfully within the payer space isn’t flashy, it’s operational. That’s a good thing. It’s about improving speed, precision, and visibility in areas that are often manual and repetitive.
Consider tasks like:
- Searching large directories for hard-to-find providers or specialties
- Summarizing unstructured data, like provider comments or survey responses
- Structuring free-text into usable data fields
- Preventing duplicate form submissions or mailings
These are the kinds of pain points AI can solve with minimal risk. They don’t make decisions on behalf of clinicians or affect member health outcomes. They reduce friction in the system, and that’s where real readiness starts.
The risk spectrum: a practical framework for AI adoption
When we talk about AI readiness, the conversation often gets polarized—either it’s full-speed-ahead automation or a complete standstill. But there’s a more practical approach, especially for provider network operations. Not all AI use cases carry the same level or complexity or risk, and that’s where a structured framework helps.
At Andros we think about AI readiness not as a binary, but as a spectrum—from low-risk, high-confidence applications to high-risk, high-stakes scenarios that require greater oversight. This framework helps health plans identify where to begin, how to experiment safely, and how to scale AI use responsibly over time. It’s not just about what AI can do, it’s about what it should do first based on your goals, workflows, and appetite for change.
Here’s an example of how we break it down:
| Low-risk (where to start) | Medium to high-risk (where to use caution) |
|---|---|
| These use cases are familiar, auditable, and easily monitored—making them ideal for teams who want to explore AI without upending existing workflows | These use cases are more complex and require mature governance—they’re not off the table, but they’re not the starting line |
| Information retrieval identifying network gaps or adequacy blind spots | Predictive modeling tied to member outcomes |
| Summarization and categorization surfacing common provider feedback themes | Automated decision-making around access, cost, or routing |
| Automation of rigid tasks form population, data validation, ticket routing | Unmoderated communications form involving PHI or sensitive data |
How to experiment safety
As provider networks grow more dynamic, the old way of managing them—manual spreadsheets, reactive planning, disconnected systems—aren’t enough. AI can help teams stay ahead, but only if it’s applied with care.
The key is to use AI where it helps people do their jobs better:
- Give teams quick insight into recurring issues
- Help credentialing teams reduce form errors or find missing information faster
- Make network development teams more agile by accelerating search and analysis
These aren’t speculative future-state goals, either—they’re things health plans can and should be doing today.
Andros Arc™ is an AI-ready platform
AI readiness isn’t just a concept we talk about, but a capability we’ve built into the foundation of Andros Arc. Arc is designed to help health plans start where it makes the most sense, with low-risk, high-impact AI use cases that enhance human performance, improve accuracy, and streamline operations. Our approach supports AI integration that is safe, scalable, and designed for real-world workflows.
For example, Andros Arc can listen for a diagnosis update, summarize notes from a referring provider, run a provider graph lookup for matching specialists, and generate a recruiter ticket in Salesforce, as the workflow below illustrates.
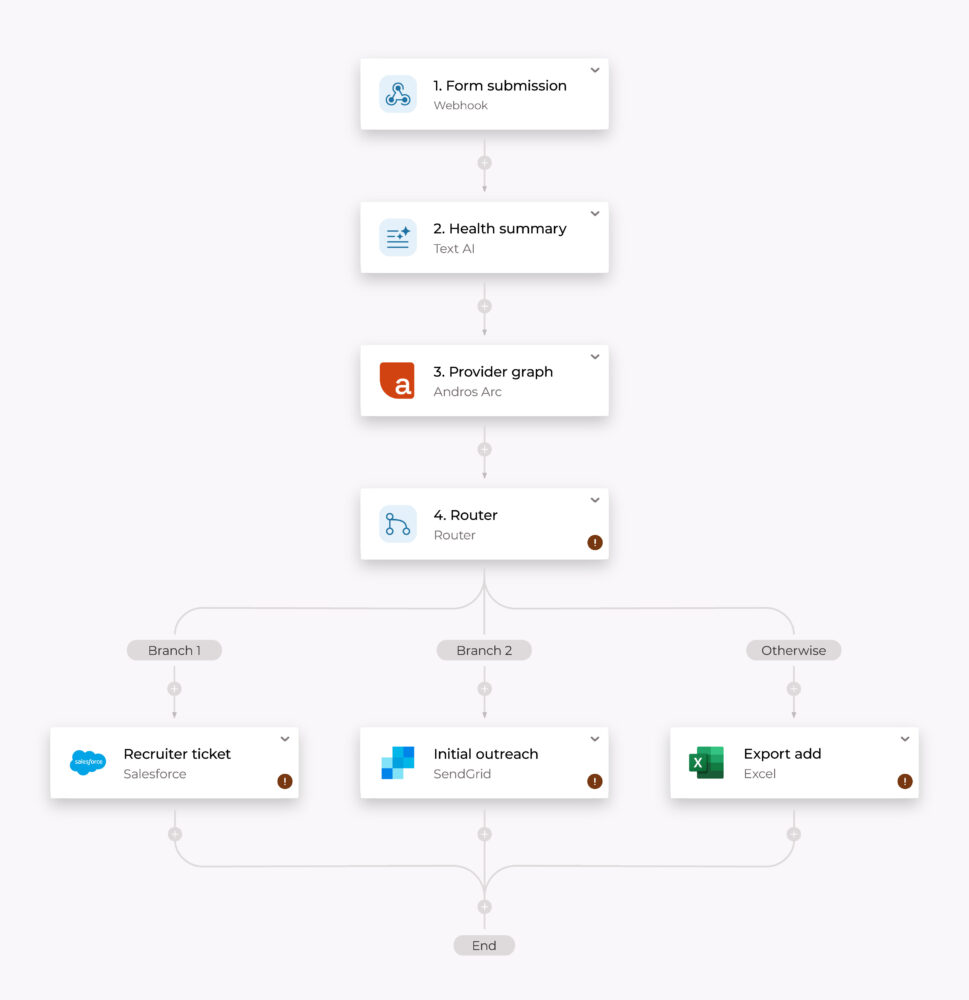
Andros Arc supports AI readiness in a number of ways, from the example above to:
- Operational AI, built in: From search and summarization to task routing or ticket creation, Arc uses AI to help teams work faster and more precisely without replacing human oversight
- Embedded guardrails: Every AI-enhanced process in Arc is designed to include checkpoints, audit trails, and human validation where needed, so teams stay in control
- A platform that grows with you: We’re focused on the left-hand side of the AI readiness spectrum where risk is low and the return is real, but as your organization gains confidence, Arc is ready to support more advanced AI use cases down the road
With any AI strategy, readiness doesn’t have to mean a complete transformation on day one. It means taking smart, practical steps that build momentum and deliver value.
If you’re exploring AI readiness in your provider network, we’re here to help. Andros Arc is purpose-built to support health plans at every stage of the journey—from first experiments to scaled impact.
Reach out to learn more about how Andros can help your team work smarter with AI.