Since its launch by CMS, Medicare Advantage (MA) has transformed healthcare in the United States. As a result, Medicare beneficiaries now have more options and insurers are competing on price and quality, which has led to lower healthcare costs and better healthcare outcomes.
It seems like a win-win scenario for health plans and consumers… until you recognize which group is being ignored in the calculation: providers. Healthcare providers are often requested to join multiple Medicare Advantage networks as health plans compete to strengthen networks in existing markets and enter new ones. It’s overwhelming. Rather than feeling like skilled, trained, caring providers, they may start to feel like a commodity. And as a consequence, providers lose interest in joining, or remaining in, provider networks—even the good ones, including yours.
How do you cut through the noise and truly stand out? It starts with understanding what motivates providers to participate in a healthcare network.
What matters to healthcare providers
With more invitations to join networks than they care to accept, providers can afford to be picky. So if you’re looking to build a Medicare Advantage network, you need to deliver what matters to them and communicate it quickly and clearly. Some of the most important factors influencing provider enrollment decisions include:
Reimbursement rates: Providers want to be fairly compensated for their services, and health plans that offer competitive rates are more likely to attract the most desirable and in-demand providers.
Claim payments: Another factor that influences provider decision-making is the accuracy and timeliness of claims payments. Providers would rather work with health plans that have a track record of paying claims accurately and promptly. You better believe that word gets around if getting paid is a headache.
Administrative burdens: Healthcare is always going to have a certain amount of administrative burden associated with it–but no one likes it. Providers prefer health plans that have streamlined and modernized administrative processes, from enrollment and credentialing to pre-authorization and payment.
In-network hospitals and health systems: Providers want to work with health plans that have established relationships with their preferred hospitals and health systems. They need to trust that when they refer a patient for specialized subspecialties or hospital care, the patient is getting the care they need promptly, from well-qualified providers.
Representatives and responsiveness: When providers reach out to a health plan, they—like any other customer—want to feel like their concerns or questions are being dealt with by someone who cares and is empowered to provide resolution. That might mean having individual representatives dedicated to specific regions or setting and enforcing standards for timely responses.
Other factors: Not every provider will make decisions based on the same factors or weigh the above factors the same way, but other elements that can influence providers’ decisions include current membership in the market, brand recognition and reputation, product lines (Medicaid, Medicare, or commercial), and payment models (e.g., value-based contracting or pay-for-performance).
How provider data improves healthcare network development
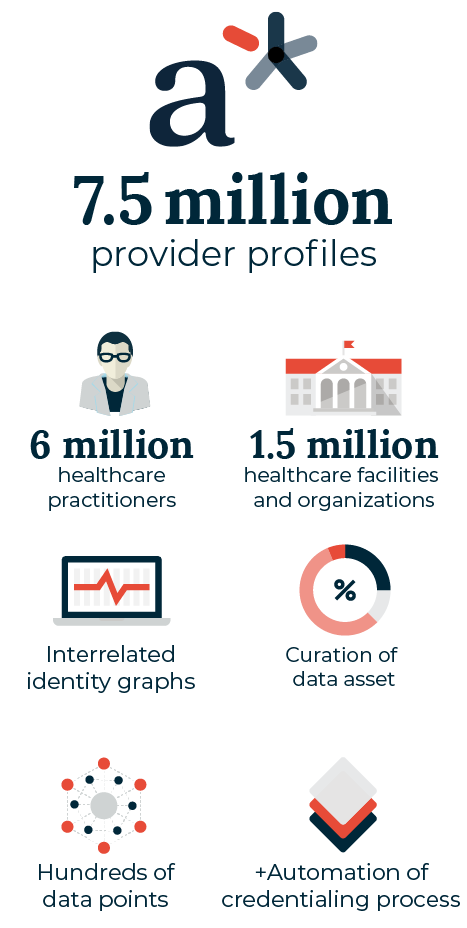
As in so many other industries, the ability to collect, interpret, and act on data quickly can lead to better decision making, product delivery, and achieving organizational goals. In healthcare, the most critical data set that can help health plans build better Medicare Advantage networks faster is provider data—and andros has the most comprehensive provider database with hundreds of data points on 7.5 million healthcare providers across the United States in the a* platform. andros leverages this wealth of data across the entire Medicare Advantage network development process, helping our clients achieve their goals, whether they’re building new networks or maximizing the marketability of an existing network in today’s competitive marketplace.
At the start of the process, andros uses this data—and our experience building Medicare Advantage networks across the country— to explore various contracting groups and provider specialty types combinations available within a market. Once we engage with a client, andros leverages smart recruiting to build a plan and strategy to efficiently achieve your network composition objectives. Utilizing different low- and high-touch methods of contact with providers, allows andros to recruit and contract providers more efficiently than standardized, ineffective, mass communications. Past experience and an understanding of critical provider networks and facilities in a given geography allow andros to prioritize and segment outreach to providers for efficient recruiting and contracting. This approach is known as “the fastest path to adequacy.”
andros tracks the results of our engagement and contracting throughout the Medicare Advantage network development lifecycle, recommending adjustments to the approach and increasing the marketability of contract offerings based on the signals received from providers. Are reimbursement rates generating pushback? Are providers responding well, providing an opportunity to develop a more competitive network in the geography? By continuously measuring performance against objectives and modeling scenarios for the future, andros offers insights on rates, language, and other contract components to improve results.
Medicare Advantage network development doesn’t end with CMS approval. In terms of actual impact on health outcomes, it’s just the starting point. And it’s also just the beginning of what andros can offer in terms of value. andros delivers a contracted and credentialed network, can monitor networks to ensure ongoing compliance, and even expand the provider network to increase its marketability and market share.
The andros difference in provider network development
The stakes are high in developing a new provider network, which is why andros works so closely with its clients throughout the process. andros isn’t just a vendor. Our data offers deep insights; our technology delivers industry-leading efficiency; and trained recruiting and contracting specialists function as an extension of our clients’ network development teams to consistently and accurately deliver the value proposition and benefits providers gain from their participation in a network. We not only communicate these benefits, but we also relay the urgency of the request to join a new network. Our objective is to simplify the process of recruiting, enrolling, and credentialing for providers. We have earned a reputation for being highly responsive, knowledgeable, and efficient in clarifying timelines, requirements, and the necessary steps for achieving a successful contract execution. Our best-in-class data, technology, and service drive results for our clients, creating a foundation of confidence and trust between the provider office and health plan that promotes long-term results for patients, providers, and health plans alike.

Find out more about network development at andros here.

