Cloud-based Credentialing CVO for Sanford Health Plan
The Next Wave in Provider Credentialing
Eliminate antiquated processes and drastically reduce the manual labor and operating costs typically necessary for provider credentialing by combining the power of the healthcare industry’s largest provider data platform with our NCQA-Certified CVO team.
You get the speedy, error-free results you need, all without looking at endless spreadsheets and paper forms.
See andros credentialing in action at Sanford Health Plan.

How andros credentialing works:
We take the manual burden off your team and help you streamline processes, reduce overhead, and increase data accuracy with our cloud-based platform.

A Simple Application Process
Our application system is designed to make providers happy by providing a robust repository of data that helps autofill provider information from verified sources.

Automated Primary Source Verification
Data-matching algorithms can help with primary source verification, identifying information gaps, and flagging potential roadblocks to credentialing, such as malpractice, licensure, or sanctions issues.

Trained Professional Oversight
Our application system is designed to make providers happy. We receive your data through an API, batch upload, or the provider-filed application, which triggers the process and alerts andros to identify the data required to complete an NCQA-certified credentialing process.

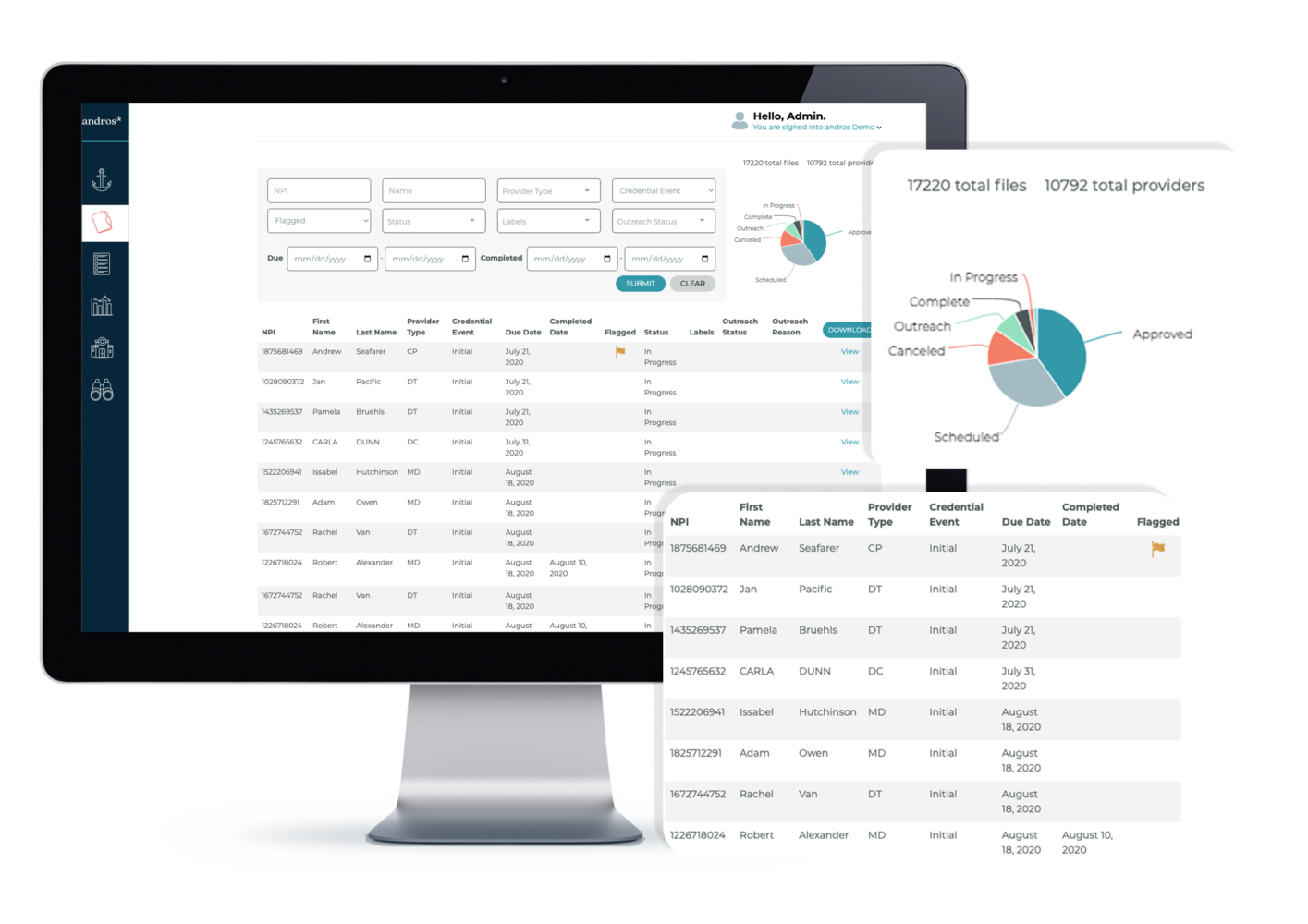
All Provider Data, At Your Fingertips
Receive all the provider information in an easy-to-read profile, including vital information like specialty, languages, malpractice information, credentialing status and much more.

An Approval Process Your Team Will Approve
Receive all the provider information in an easy-to-read profile, including vital information like specialty, languages, malpractice information, credentialing status and much more.

Credential with ease. Eliminate redundancies, inefficiencies, and errors.
The a* platform aggregates and re-uses provider data to eliminate redundant steps in the credentialing process. We set up our best practices to ensure transparency, workflow management, and accountability.
- Complete routine tasks accurately and efficiently.
- Start credentialing when providers are engaged.
- Minimize the risk of getting approved, but not in-network for open enrollment season.
NCQA-Certified credentialing for over 7 million healthcare providers, and counting.

Industry-leading Turnaround
The andros a* platform enables credentialing workflows up to 10 times faster than industry averages. Light years ahead of the market, our credentialing service reduces overhead and ensures accuracy every step of the way. andros clients experience industry-leading turnaround times on thousands of complete files. In addition to primary source verification, we also offer monitoring and network approval management services.

Fully NCQA-Certified CVO
Our platform offers the strictest level of NCQA certification available. With such rigorous standards applied to every file, we drastically reduce errors and audit risks — so you can be reassured that your network quality is exceptional. Combining speed with NCQA certification ensures that credentialing meets the needs of health plans, providers, and ultimately patients.
Dramatically Improve Efficiency
Through data intelligence and automation, androsCredentialing* removes manual work, greatly reduces admin times, and creates efficiency never before found with credentialing processes. As a result, andros can give you an ROI of 300% or more on credentialing services compared to fully staffed internal teams using in-house data systems and traditional manual workflows.

Humana proactively identified and mitigated potential compliance issues
Humana achieved 94% file completion before the due date, a 32% improvement from previously.

PPHP cut down their credentialing time from several months to just days
With andros credentialing, PPHP reduced their credentialing time to 10 days.
Modern CVO
Credentialing At Scale
By leveraging our cloud-based platform and deep provider data in the a* platform, we can credential thousands of provider applications far faster than in-house teams or other CVOs. If you’re ready to see how you can get speedy, error-free results without looking at endless spreadsheets and paper forms, request a demo.